1. Post-operative Trauma Follow-up Assessment
:
Run based on which sequence(s) the pathology has been previously best seen.
:
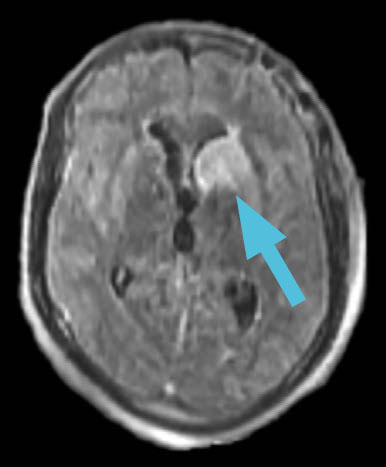
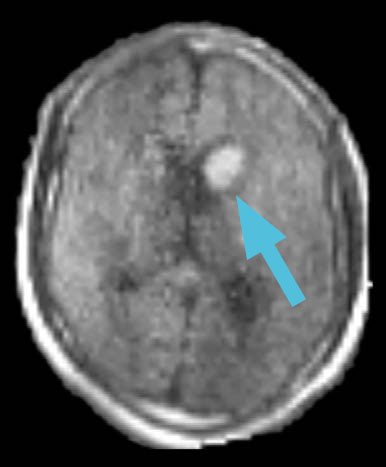
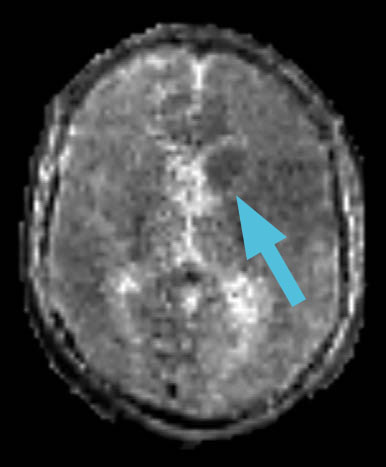
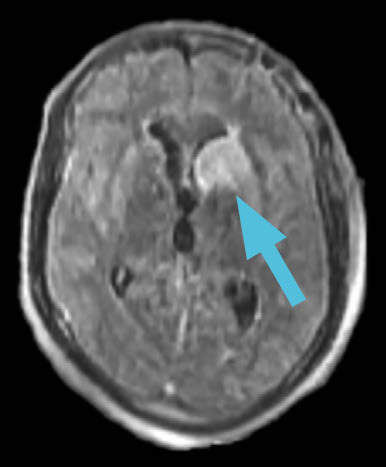
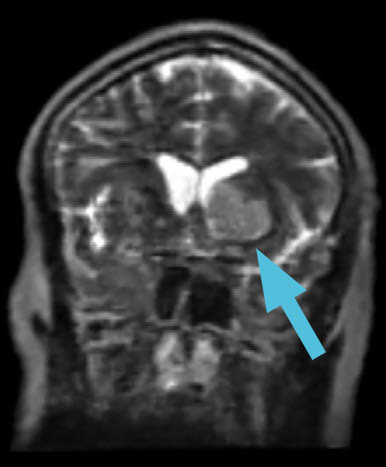
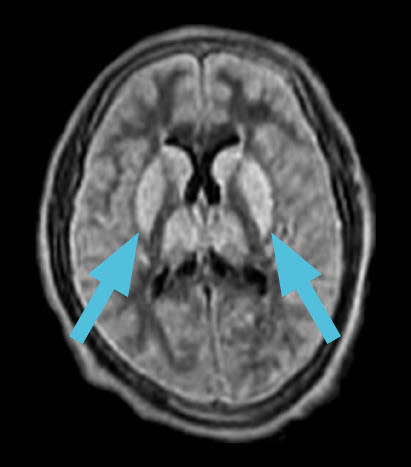
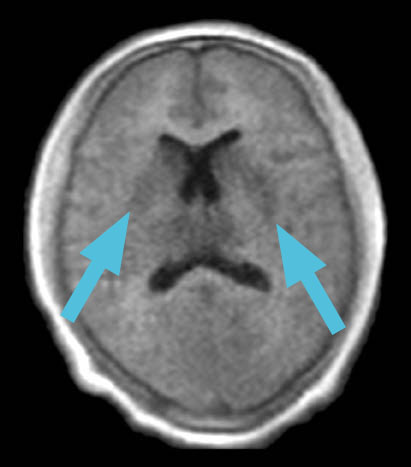
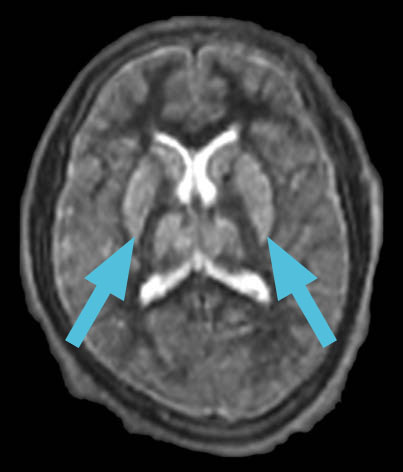
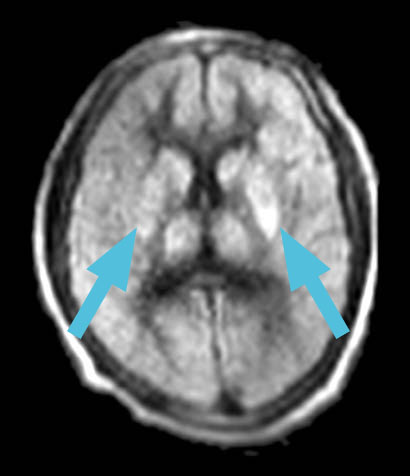
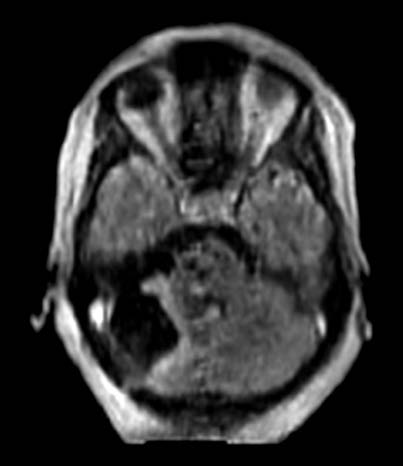
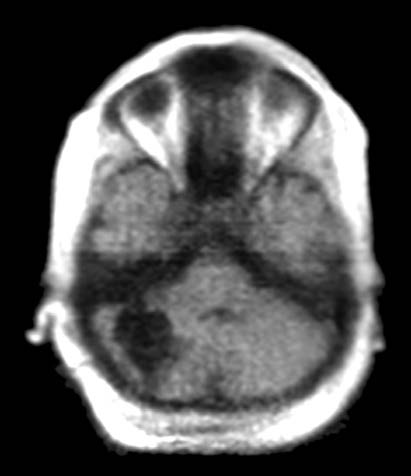
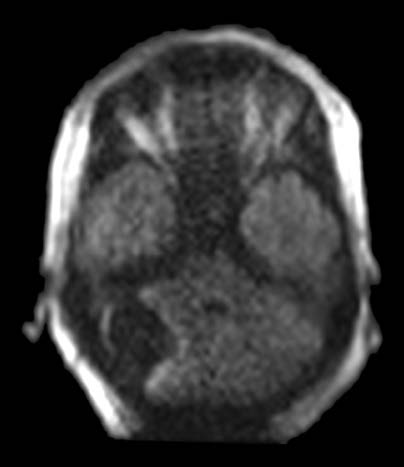
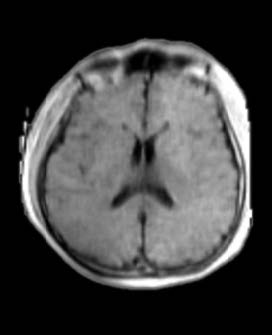
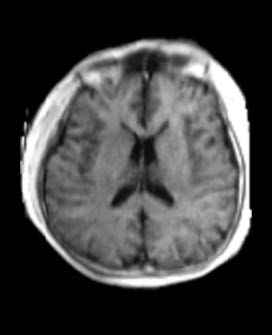
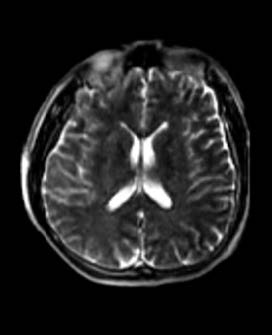
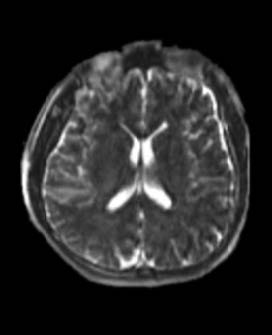
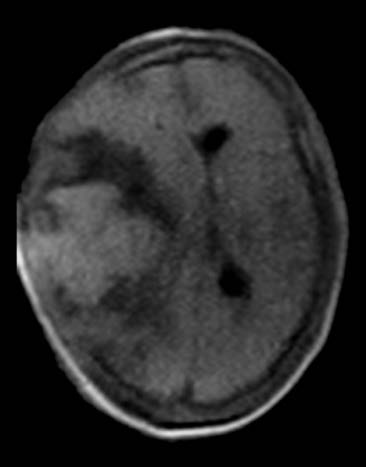
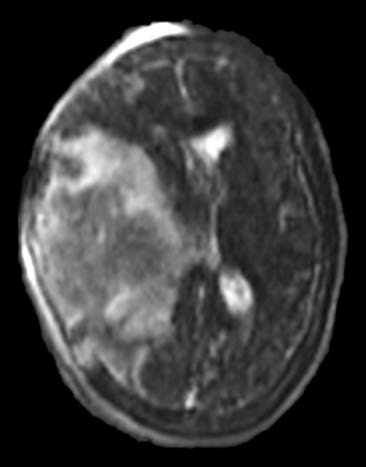
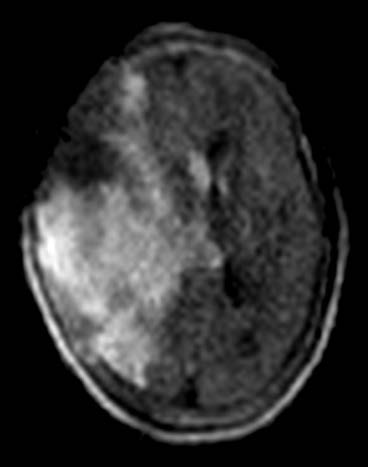
A 35-year-old female found unresponsive was brought into the emergency room. An emergent head CT revealed a massive traumatic intraparenchymal hemorrhage. Clinicians immediately took the patient to the operating room for decompression.
:
Post-operatively, physicians used the Swoop system at the patient’s bedside. The images assisted them in assessing the extent of mass effect, midline shift, and tissue viability for prognostication.
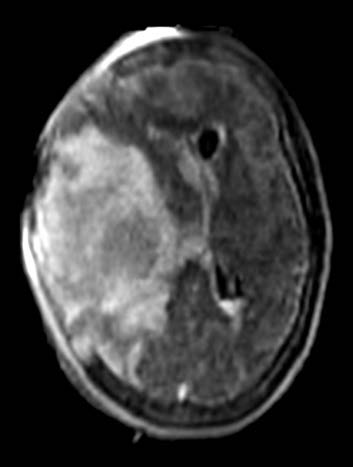
The Swoop system is not intended to apply color overlays to images. Colors are added for clarity and are not reflective of the original images.